- Researchers estimate that about 22% of all adults aged 50 and above globally have some stage of Alzheimer’s disease.
- Researchers are focused on finding new ways to recognize early warning signs of Alzheimer’s disease as medications can help at the earliest stages.
- Scientists from the Johns Hopkins Bloomberg School of Public Health found that monitoring a person’s daily activity patterns through a wrist-worn device may spot early warning signs of this type of dementia.
Researchers estimate that about
With this number expected to increase, researchers are focused on finding new ways to recognize early warning signs of this type of dementia.
Although there is currently no cure for Alzheimer’s disease,
One of the latest studies on Alzheimer’s disease early detection research comes from the Johns Hopkins Bloomberg School of Public Health.
In a new study published in the journal SLEEP, scientists found that monitoring a person’s daily activity patterns through a wrist-worn device may spot early warning signs of Alzheimer’s disease.
Each day, most people have a set pattern or routine of certain behaviors, including activity. For example, some people may be more active in the morning while others move more in the evening. This is known as a person’s daily activity pattern.
Past studies have linked a consistently highly active daily activity pattern with a healthier
Researchers have also linked a regular daily activity pattern to
A study published in May 2018 reported that daily activity patterns of older men may be predictive biomarkers for changes in clinically relevant outcomes for mortality, as well as changes in sleep and cognition.
And research published in October 2019 found that a more
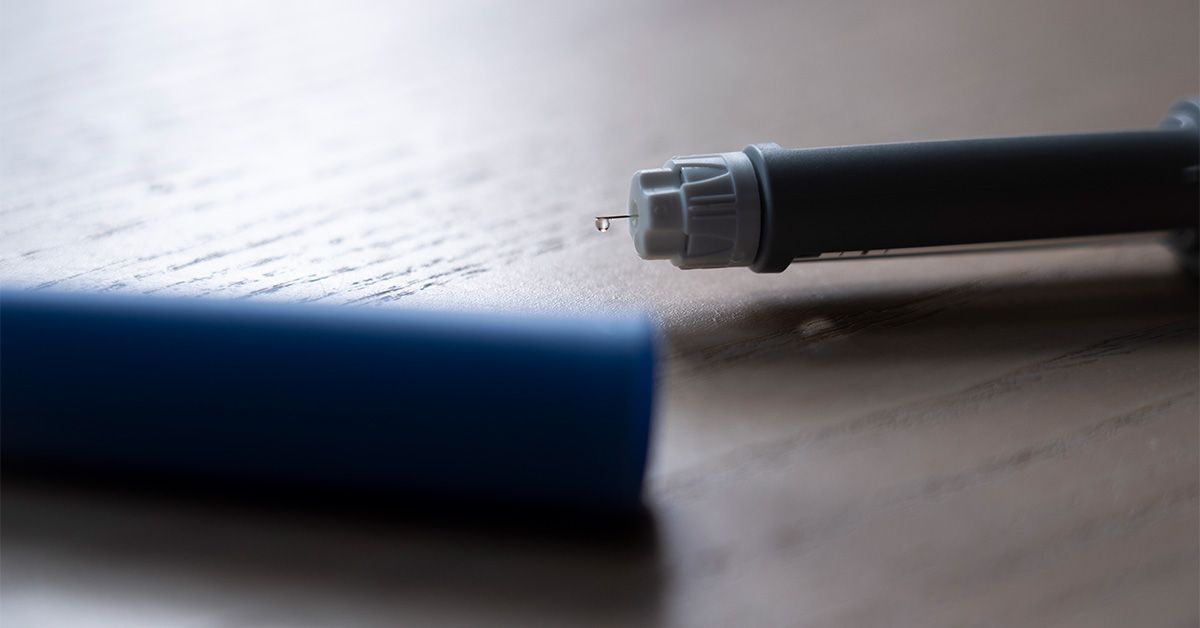
For this study, researchers studied the data produced by a wristwatch-like device called an
“For decades now, sleep researchers have used wrist-worn actigraphs to study sleep in older adults,” Dr. Adam Spira, professor in the Department of Mental Health at the Johns Hopkins Bloomberg School of Public Health and lead author of this study, explained to Medical News Today.
“The technology — typically an
“Because of growing evidence that
Of the 82 study participants with an average age of 76, some had detectable amounts of the protein
When analyzing the data collected by the actigraph devices, the researchers reported significant differences between the 25 “amyloid-positive” and 57 “amyloid-negative” participant groups in average activity during certain times in the afternoon, as well as differences in the variability of activity throughout the days during a broader time window.
The scientists discovered those in the “amyloid-positive” group had higher average activity during the early afternoon (1:00 p.m. to 3:30 p.m.) and fewer day-to-day activity changes from 1:30 to 4:00 p.m. and 7:30 to 10:30 p.m.
“Our results are noteworthy because they showed, in people who were cognitively normal, that those with detectable beta-amyloid in their brains had different patterns of activity at particular times of day from those without beta-amyloid,” Dr. Spira said. “This is a novel finding.”
“It will be important to follow people who exhibit patterns of activity like those that we linked to the presence of beta-amyloid, to see if they are at greater risk of subsequent cognitive decline,” he continued. “It would also be intriguing to examine whether these 24-hour patterns predict the development of beta-amyloid in those who do not have it.”
While in this study researchers used a scientific-based wristwatch-type device, would people one day be able to detect early warning signs of Alzheimer’s disease through mainstream fitness and activity trackers like Fitbit, Garmin, and the Apple Watch?
At this point, Dr. Spira said people should not try to interpret data from their own devices as a sign of whether or not they have amyloid in their brains.
“Whether these methods could be used in the future for early detection of Alzheimer’s disease depends on whether further studies support our findings or identify other ‘digital signatures’ of Alzheimer’s disease that can be detected using wearable devices,” he explained.
“If they do, it is conceivable that one day, wearable devices will be used to help identify people at elevated risk for neurological disorders like Alzheimer’s disease. We’re not there yet, though,” Dr. Spira cautioned.
After reviewing this study, Dr. Clifford Segil, a neurologist at Providence Saint John’s Health Center in Santa Monica, CA, not involved in the research, admitted to MNT that he was confused by the study, as Alzheimer’s dementia is a memory loss disorder and not a movement disorder.
“The data supports that the older adults in this study who were amyloid-positive moved better during the early afternoon and had less movement variability in the late afternoon and evening,” Dr. Segil explained.
“I think the authors are trying to provide a framework to look at ‘
sundowning ,’ which is a phenomenon when patients with Alzheimer’s Dementia become more agitated at night. I am assuming an agitated old adult would have higher movement variability than a non-agitated older adult.”– Dr. Clifford Segil
“I don’t think a wearable recording ‘wrist actigraphy’ will be used clinically in the diagnosis of a memory loss disorder like Alzheimer’s dementia in the future,” he continued.
“Decreased activity as people age is normal and more worrisome for other medical comorbidities like heart disease,
MNT also spoke with Dr. Jennifer Bramen, a senior research scientist at the Pacific Neuroscience Institute in Santa Monica, CA, who commented it is too early to conclude if the study’s finding is specific to Alzheimer’s disease or indicative of another overarching condition, such as a sleep disorder, which is common in Alzheimer’s patients.
“It might be valuable to conduct similar research on individuals with and without sleep disorders to assess the potential of this technology in detecting conditions like sleep apnea,” Dr. Bramen continued. “This is because it is a common occurrence and is a well-established modifiable risk factor for heart disease, stroke, and Alzheimer’s disease.”
“I would be skeptical of utilizing wrist-worn devices for detecting Alzheimer’s disease,” she said when asked if people may be able to use mainstream fitness trackers to detect early warning signs of Alzheimer’s disease in the future.
“These devices can make mistakes, potentially causing unnecessary distress and burdening the medical system with unwarranted testing for well patients, while possibly delaying diagnoses for truly impaired individuals,” the expert cautioned.